Think of a situation where you are rushing for a school meeting of your daughter, only to find the need to rush back home, as the pressure of urinary bladder could not be controlled. A handful of women turn out to blame nature on the second level rather than seeking gyanecologist's or urologist's help. An investigation done by the Indian Journal of Urology shows that about 40 per cent of Indian women above 40 have urinary incontinence, while less than two per cent actually consult the doctor.
Urinary incontinence is involuntary leakage of urine and can affect women of all ages in India, from young mothers after pregnancy to older women. Many women live in silence with this condition, viewing it as part of aging or feeling too embarrassed to talk to family members or family doctors.
In the following guide, we will learn about the beginning signs of urinary incontinence in women, their types, the common causes, and their treatment options.
What are the first signs of urinary incontinence (UI)?
It is important to recognize the signs of urinary incontinence before it is too late to intervene. One of the first warning signs is when you laugh, cough, or sneeze, and a few drops of urine leak.
You may also notice a dampness in your underwear after lifting heavy objects or during your morning strolls. Some women have a sudden, intense urge to urinate that may make it challenging to reach a bathroom in time.
Other early warning signs include frequent urges to urinate during the night (nocturia) and a feeling that your bladder is still full, even after going to the washroom. These behavioral changes, such as planning your day with bathroom locations in mind or cutting back on your intake of fluids, are significant to make a note of.
For some women, the change occurs during pregnancy or immediately after birth; for others, it occurs around menopause.
Also read: Remedies to cure urine infection at home
Types of Urinary Incontinence
Here is a summary of all forms of urinary incontinence in women:
Stress Incontinence
This is the most common type of urinary incontinence in Indian women, especially those post-childbirth. It occurs when pressure is put on the bladder by some physical movement or activity. Simple actions like laughing, coughing, sneezing, or working out may cause leakage of urine. The weakening of pelvic floor muscles during pregnancy and after childbirth makes urination control difficult. Many women experience this when doing housework such as lifting heavy objects or even during their morning walks. The amount of leakage that an individual has is usually minimal, ranging from drops to a small stream.
Urge Incontinence
Also called "overactive bladder", you might find it difficult to manage the sudden and strong urge to urinate. Often the urgency and subsequent leakage are provoked by simple stimuli, such as hearing running water or entering the house. Many women suffering from this disorder tend to mentally map out toilet locations wherever they go. It might feel like the urge is so sudden and powerful that urine is released before making it to the toilet despite a full, somewhat filled, bladder.
Overflow Incontinence
Overflow incontinence occurs when the bladder does not empty completely when urinating, thus leading to leakage due to prolonged dribbling. Women suffering from this type commonly notice that their bladders never seem to fully empty, even after going to the bathroom. You may have many small leaks during the day or have a weak urine stream that stops and starts. This type is common among women due to diabetes or nerve disorders affecting the bladder nerve signals.
Mixed Incontinence
This type of incontinence is a mix of the two groups of incontinence, i.e. stress and urge. There may be functional leakage, that is, the leaking of urine in the active state, like when one is playing; along with in this, there comes the urgency of desire to urinate, like urge incontinence. The dual character accounts for its difficult management. Reflex incontinence requires a combination of treatments to learn to address its symptoms effectively.
Total Incontinence
Total incontinence is the worst form of incontinence where one is leaking urine all the time and unpredictably has episodes of massive leakage within a short duration of time. Women with this condition may have little to no control over their bladder, requiring constant protection. This kind of incontinence is often a result of serious underlying conditions, such as fistulas, neurological disorders, or prior pelvic surgery. Totally incontinence affects a person's day-to-day work and mandates immediate medical attention for their proper management.

Common Causes and Risk Factors
- Age-related factors
- Pregnancy and childbirth
- Menopause
- Medical conditions
- Lifestyle factors
- Cultural Practices
Age Factors
As women age, their muscles supporting the bladder usually become weaker. In older women, elasticity of bladder tissue is lost, leading to diminished bladder capacity and more possibilities for urinary incontinence. The amount of urine left in the bladder after urination also tends to increase with age. This natural aging process, together with hormonal changes, renders women over the age of 50 most prone to urinary incontinence.
Pregnancy and Childbirth
During pregnancy, there is constant pressure on the bladder from the enlarging uterus, and hormonal changes affect bladder control. Vaginal delivery can weaken pelvic floor muscles and may affect the bladder directly in some women through direct nerve injuries or damage to the support tissues. The risk is heightened with multiple pregnancies and deliveries. Most Indian women may have extended effects on bladder control due to undermined pelvic floor rehabilitation after delivery, especially for those with home deliveries or having had limited care.
Menopause
The significant drop in estrogen levels during menopause affects the lining of the urinary tract and the pelvic floor muscles. These hormonal changes may mean less control over the bladder and frequent urination. Many Indian women going through the menopause may consider this as age-related and not realize that hormonal therapy replacement or other therapies exist to treat those symptoms.
Medical Conditions
Some medical conditions that may lead to urinary incontinence:
- Diabetes, affecting nerve function
- Urinary tract infections (UTIs)
- Hysterectomies or other pelvic surgeries
- Neurological disorders such as multiple sclerosis
- Chronic cough due to a respiratory disorder
- Obesity, which presses on the bladder
Lifestyle Factors
Diet and lifestyle factors directly affect bladder control in many different ways: Excess consumption of caffeine or spicy foods, insufficient water intake owing to leakage fears, lack of exercise leading to weakening of pelvic muscles, constipation owing to excess pressure on bladder, and smoking relating to chronic cough with corresponding straining. You can read our detailed blog on foods to avoid during periods.
Managing and Treating Urine Incontinence (UI)
Treating urinary incontinence takes a combination of medication and lifestyle adjustments. Your doctor may recommend medications to help with overactive bladder and urgency, while much more serious cases may require minimal surgical procedures to support the bladder and give long-term relief.
Ayurveda offers several natural cures for urinary incontinence. These age-old Ayurvedic treatments help to support modern-day medical therapy. Similarly, homeopathic medicines provide some mild alternatives for the treatment of incontinence symptoms, especially for women looking to gain the benefits of natural treatment.
Kegel exercises are highly important to aid in strengthening the pelvic floor muscles that keep one from urinating. The exercises can be easily undertaken anywhere-in the kitchen, while watching TV, or even during prayer. Simple yoga postures have been known to work fairly well in maintaining bladder control.
Homeopathic treatments for Urinary Incontinence (UI)
Urinary incontinence can be very frustrating, but homeopathy has a gentle and effective way to treat this ailment. Certain homeopathic remedies like Causticum, Sepia, and Kreosotum are used, depending on the clinical picture presented by the patient. As each woman's body responds differently, it is highly recommended to consult a qualified homeopathic doctor before considering any remedy. He or she would assess your condition and prescribe the most suitable treatment.
Lifestyle changes and modifications
Lifestyle changes influenced by bladder function can offer relief in other ways, including:
- Weight control
- Bladder-friendly diet
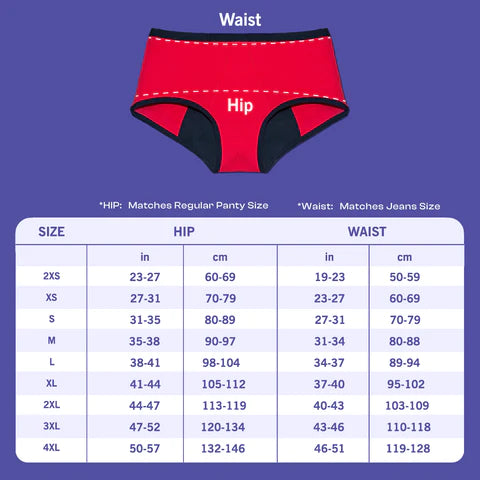
- Wearing Period Underwear for Urine Incontinence
- Avoiding bladder irritants such as caffeine, alcohol, and spicy foods
- Drinking plenty of fluids instead of limiting fluids to cut back on bladder activity

When to consult a doctor or urologist
While some of the urinary problems may be minor, the following symptoms require immediate medical attention: Red flag symptoms include:
- Blood in urine
- Unexplained weight loss
- Severe pelvic pain
- Repeated urinary tract infections
- Total inability to empty your bladder
- Sudden onset of urinary problems
- Persistent fever along with urinary symptoms
Gynecologists or urogynecologists can be consulted for urinary incontinence issues. Look for experienced specialists in treating female urinary health issues. Many hospitals have established women's health clinics where you can feel free to share your concerns in major Indian cities.
Key takeaways
So, there you have it! This guide has given you an introduction to urinary incontinence in women, its causes, symptoms, and possible treatments including homeopathy. We hope this gives you an adequate overview for understanding the condition and for being able to make better-informed treatment decisions. Please remember that each woman's experience is unique, so the best course is to always consult a professional health worker to put forward an effective treatment plan accordingly.